The PBF Community of Practice has initiated a collaborative learning program on ‘PBF & Quality of Care’. Health Financing in Africa welcomes testimonies, opinion pieces and presentations of research findings. In this second blog of our series, Peter Eerens shares his own 30-years journey on quality improvement.
This is not a review, but the recollection of a journey with quality improvement.
In living health systems, all elements connect with several other health systems parts. Interdependence characterizes their joint timewise evolution. No part of a health system is ever final, finished, or perfect. No country has the health system it ultimately wants. Our insights in systems and system dynamics help in understanding that finances, infrastructure, supplies, human resources, service delivery etc. are necessarily connected and that values, principles, policies, quality, accessibility, etc. co-constitute these evolving health systems’ networks of networks. There is nothing outlandish in stating that these constantly rewiring dynamic systems have massive links with nodes or networks in other systems (educational, economic, trade, transport systems, just to mention a few). And yes, ecology, climate, planetary survival etc. all have links with such health systems. Sounds like big thinking? No. That is what we mean by systems thinking.
From not much to checklists for supervisors
So how do we link PBF with quality, and how can we get a sense of the “quality improvement journey” in a fashion that is reminiscent of how PBF pioneers evolved a set practices that constitute today an impressive body of experience?
I remember the eighties, a time when one could make statements about quality of health services without referring in any way to quality assurance or quality improvement concepts: recruiting the right people, ensuring that adequate equipment and infrastructure was available, and providing them with supplies and appropriate funding, were considered the essential requirements for the provision of quality services. Quality was just another attribute of health services that could be “engineered” by ensuring the availability of the right inputs, very much like we looked at availability, accessibility, affordability, continuity, or integration, i.e. attributes that came into being by “doing things right”.
More than thirty years later, does one still hear such statements? Not really. Health systems managers have embraced management cultures in which quality improvement is part and parcel of established managerial techniques. Although...! In 2014, I asked a few experts which quality improvement system was in place to achieve the health services quality goals of their country’s health sector development plans. “No... No special interventions. That’s just a matter of getting the inputs in place”. The answer made perfect sense to me. Health systems have diverse histories and no history is intrinsically “better” than any other.
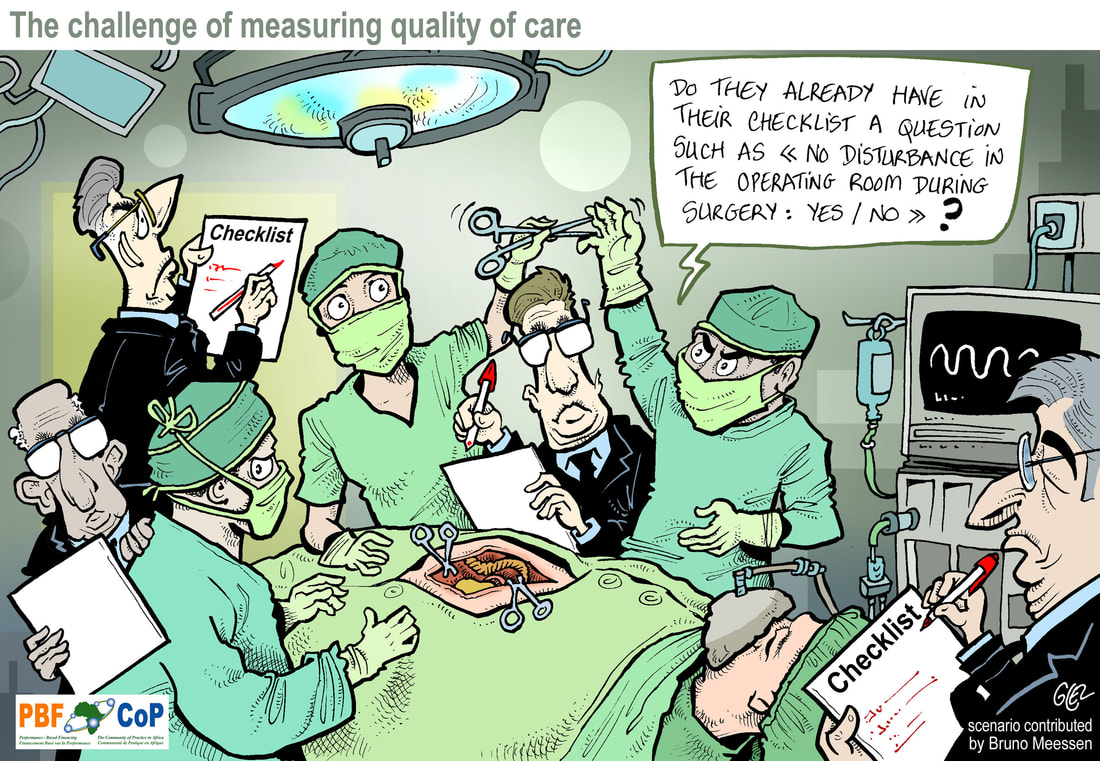
In those earlier years – focused on primary health care - we also thought that supervision was the process by which we could ensure progressive improvement of the quality of services. I remember very well how one of our supervisors attended a national level training and returned with a set of large folders on supervision and …checklists. Unaffordability of paper, in amounts needed to manage these checklists, would be the main implementation obstacle for our resource constrained district office. We re-invented thus the “checklist”, and designed a decimal system based catalog of binary evaluators which reduced our paper needs dramatically. We called it the Maendeleo Score, to honor the supervisor who was part of its design. This was the period when integrated circuits were the talk of the day and it will thus surprise no one that the similarity of our yes/no checklist with electrical diagrams of binary on/off switches made us confident we were close to fully understanding the mechanics of quality improvement processes: just a matter of getting the switches ON.
Supervision and checklists have been twin concepts ever since. But who hasn’t come across the massive amount of data stored in such printed forms, unexploited and unexploitable? Indeed, apart from generating data for immediate local use, supervision checklists produced massive amounts of multidimensional information, for which no data processing tools were available. Nevertheless, supervision checklists remained an essential element in the district toolbox. They started to change our way of thinking about data, information and networks.
Emergence of quality assurance programs
Our fascination with checklist was genuine, but very soon we were told to think differently. Other winds crossed the traditional oceans. Established quality assurance practices from the manufacturing and engineering industries, and to no lesser extent from hospitals in the health care industry, inspired players in the international public health arena to tackle the quality challenges of young primary health systems along the same lines. That revolution has firmly taken root but is still work in progress.
Many quality improvement strategies of today will refer first and foremost to Donabedian’s quality improvement model (1966) in which “structure, process and outcome” were linked in a potent framework for tackling quality of clinical care. While this framework helped to systematize issues of quality in health services (notice the input/output fingerprints of early systems thinking), real quality assurance techniques would be borrowed from the other industries: e.g. root cause analysis, business process reengineering, benchmarking, fish bone diagrams, cost/benefit analysis, operations research, Deming’s quality control iteration, popularized as the Plan-Do-Check-Act cycles and different adaptations, etc. Quality assurance systems promoted by ministries of health are full of these techniques.
Many people don’t know Deming’s influence on Japanese quality culture, but the Japanese approach towards quality improvement, quality control, or quality assurance (quality experts love to celebrate the distinctions between these concepts) that resulted from it is widely recognized for its influence in industrialized countries. As such, the Toyota culture also influenced QI in current health systems thinking: 5 Whys, TQM (total quality management), 5S (the Seiri, Seiton, Seiso, Seiketsu, Shitsuke sequence that translates in the English Sort, Set, Shine, Standardize, Sustain) and finally Kaizen, which is essentially “continuous” improvement in Japanese, even when some countries speak of their “Continuous Kaizen”, to make it resonate with Continuous Quality Improvement (CQI).
Checklists were never far away from these quality improvement techniques. But just like checklists were not “the solution” for achieving quality, quality assurance models and techniques were also just the tools and not “the solution”. They only achieve full potency when mindsets are properly aligned with the promoted quality culture (see also Toyota’s slogan of “building people before building cars”).
Situation today
In today’s health systems, we encounter full hybridization of those techniques. They are promoted into national strategies through the branded contributions of multilateral organizations (e.g. Bamako Initiative by UNICEF, IMNCI Supportive Supervision Checklist by WHO), bilateral institutions (e.g. Kaizen by JICA; BPR by USAID, QIT by GiZ), universities or their affiliates (e.g. SBM-R by JPHIEGO), consulting firms (e.g. QI Collaboratives by URC); not-for-profit corporations (e.g. CQIT by Amref Health Africa; HEALTHQUAL by Health Research, Inc) or non-governmental organizations (e.g. COPE by EngenderHealth; IQMS by IHPMR).
They all have in common that they emphasize processes, iterations, trials, and … data. It is interesting to contemplate how our understanding of data has changed. The early and traditional approach in data driven operations research was to generate the data as part of the research process. Data had a price tag attached to them, and one would collect only what was needed, feasible and affordable. The fast pace of change in computerized data collection, analysis and visualization have constantly influenced this. Current information technology breakthroughs have achieved a reversal of the problem. Generating the quality data is less the problem than what to do with the wealth of data generated through increasingly prevalent data and information systems with or without the metadata generated through the mobile phone or internet based storage capabilities.
Suddenly, checklists can turn into the multi-dimensional big data gathering tools that they intrinsically are. Indeed, originally a checklist is just about “checks” as Atul Gawande describes in his Checklist Manifesto. But who hasn’t seen checklists turn into real questionnaires, and worse, supervisors behaving more like administering a survey rather than investing in interpersonal communication so dear to supervision.
A new perspective on checklists
My fascination with checklists still exists. Although I have a good grasp of all these different quality improvement techniques, of accreditation systems, of ISO certification, and although I agree with QI and QA experts that checklists are NOT that important, checklist are important to me because they provide us with the means to achieve the conceptual leap from traditional thinking about health care systems to complex systems and dynamic networks. Indeed, the binary evaluators in a checklist statement are not less than individual nodes of a binary network (the network statement would also apply if you use a Likert scale). If you are somewhat familiar with Stuart Kauffman’s Boolean systems, you see your supervision checklist turn into a network of size N, with connectivity K and with Boolean functions that govern the temporal transitions of each node as it updates itself based on the state of other nodes it is connected with. Whenever I develop this thought process for my collaborators or for a captive audience, I am surprised by the questions it generates about dynamic health systems.
It is this network thinking, with origins in plain checklist, that is at the origin of the statement at the start of this write up. The adequate counseling of a mother to monitor the temperature of her child at home (Yes/No), and the release of the quarterly funds when the health center has reached the targeted number of new mothers enrolled in the child clinic (Yes/No) are linked. It’s obvious. Quality improvement and performance based finance are linked, or can be linked if they weren’t already. And so are “The female community health worker correctly enters the date for the next family planning session for her client” (Yes/No) and “The community health worker has visited at least three households in the last week to sensitize members about tree planting” (Yes/No).
But, before we transform all these most aesthetic community health experiences in their binary information equivalents that will icloud our skies even more, I think we need to understand better how to ensure that change (from OFF to ON) in the vast micro level networks of individuals, households, villages, communities, and so forth resembles more “10010111111011101111011” rather than the less encouraging “000100001001100000000”.