In September 2018, the World Health Organization (WHO) and the African Development Bank (AfDB) organised a conference in Nairobi on Public Financial Management (PFM) in health. This conference gathered representatives from the health and finance sectors across 50 African countries, whom discussed the importance of PFM for Universal Health Coverage (UHC). Six months after, we take stock of the reform agenda and welcome your thoughts on possible ways forward. The synthesis report released this week by WHO is a modest contribution to this discussion.
More proactive engagement from health sector in PFM reform
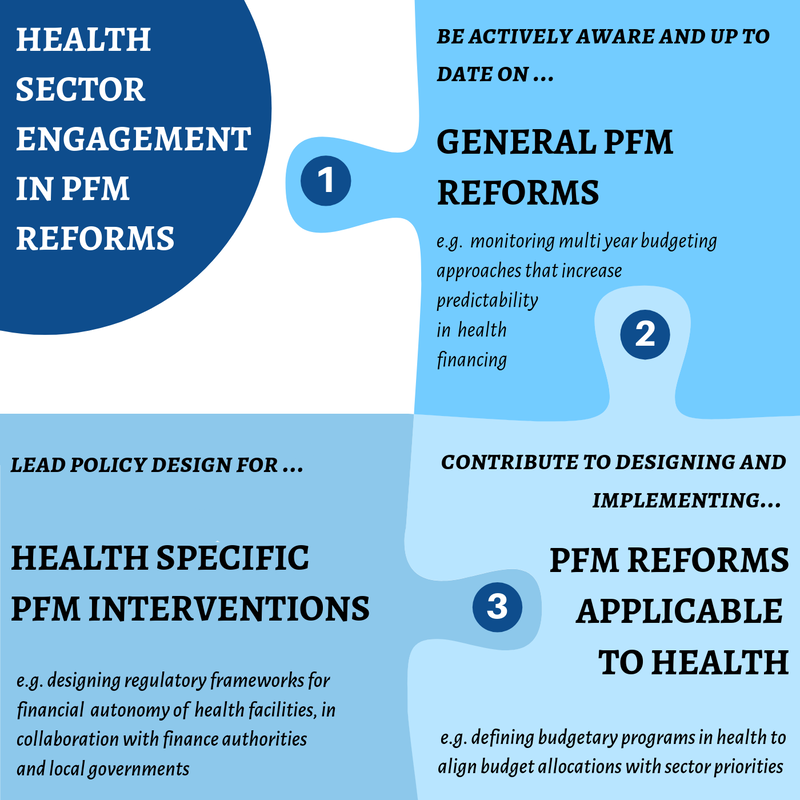
Long absent on the topic, health ministries need to take a more active role in the PFM reforms that are necessary to provide a favourable environment for UHC. Our analysis delineates three complementary areas of engagement for health ministries:
- Be actively aware and up to date on general PFM reforms (e.g. monitoring multi-year budgeting approaches that can increase predictability in health’s resources envelope)
- Pro-actively contribute to the design and implementation of PFM reforms particularly important for health (e.g. defining budgetary programmes in health that help align budget allocations with sector priorities)
- Lead policy development for health specific PFM interventions (e.g. designing regulatory frameworks for financial autonomy of health facilities).
Accelerating PFM reform implementation in health
As most African countries are halfway through their PFM reforms, they are well placed to seize the momentum and consolidate their PFM systems in order to better support progress toward UHC. Our analysis shows that implementation of the following reforms should be accelerated.
- Budget formulation: countries should accelerate the institutionalisation of programme-based budgets in health to better align budget allocations with sector priorities, provide more flexibility in health expenditure management and improve accountability by measuring resource use in relation to achieved results. In this process, the elaboration of budgetary programmes is a complex task requiring MOH’s active engagement; implementation will bring the expected results if expenditure management is no longer driven by input-based control logic and if a results-based accountability framework is in place.
- Budget execution: health budget execution is deficient in several countries. Countries should identify the root causes of deficient execution practices (e.g. funds that are badly prioritised, not disbursed on time, not flexible, under-used, wasted), in order to prioritise appropriate corrective actions. In our report, we propose an analytical framework that could guide the identification of the main causes of deficient budget execution in health, with a focus on under-spending.
- Budget reporting: financial reporting systems remain fragmented in health and are not oriented towards monitoring actual results, despite recent reform efforts. Countries are encouraged to set up a new accountability contract that enables them to consolidate and streamline the monitoring of financial and operational performance in one single framework. This is a technical requirement – for monitoring performance – as well as a commitment for citizens. By measuring the level of spending by result, the monitoring framework of programme-based budgets offer this opportunity; it should be seized.
Revising the focus and processes of PFM reforms in health
The health sector has benefited from undeniable advances in cross-sector PFM system strengthening through two decades of international support. It is time now to complement and adjust certain aspects of these important reforms by introducing more sector-specific interventions that are necessary to accelerate the PFM reform agenda in health.
The focus and processes of PFM reforms could be adjusted to better respond to the needs of the health sector. Considering some of the difficulties to implement PFM reforms in health, our analysis highlights the importance of having:
- More consideration for PFM blockages at health facility level - critical to look at the bottlenecks for accessing, using and reporting on public funds from a health facility perspective
- A deeper appreciation for increased autonomy and flexibility in financial management at health facility level - finding the right balance between the needed control of expenditure and the necessary flexibility level in using public funds according to evolving needs (e.g. change in disease prevalence, integration of new treatments, rapid response to epidemics)
- More effective coordination and consistency between PFM and other reforms affecting health spending (e.g. strategic purchasing reform, decentralization policy).
To conclude, let’s underline the urgent need to develop the technical capacities of the region in this area of work. The region needs professionals that can work at the nexus between PFM and health policy, understand both communities and can build sustainable bridges. It is a new generation of practitioners that needs to be trained, mixing skills in economics, PFM, public policies and health systems. We need you to move forward and support the implementation of this critical agenda.
You can access the new report here.