It’s striking how much the Universal Health Coverage (UHC) agenda has been, from a financing perspective, conflated with contributory health insurance. Some of the reasons are understandable. Health in many low-income countries is currently financed through a combination of tax revenue, out of pocket expenditures and donors. There is a tension between the objective of mobilizing resources for health – which suggests to maintain user fees – and the objective of access to all – which suggests to remove user fees. Many countries don’t want to lose the direct revenue from the population – pre-payment is therefore the preferred option.
I’ve been reflecting these last few months about the challenge of sub-Saharan African countries engaged in the development of some sort of (contributory) national health insurance as a means to move towards UHC. My assessment is that developing a national health insurance scheme is a challenge, not necessarily because managing such a scheme is complicated and administratively burdensome (although that is certainly true) but because of the prevailing approaches to setting it up.
The classic sequencing approaches
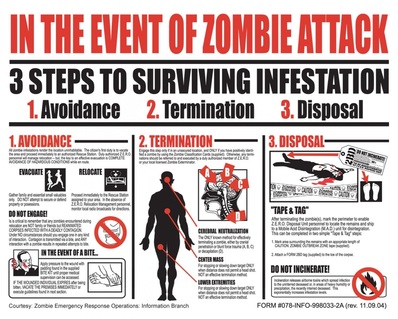
I have observed three approaches for sequencing the setup of national health insurance: (i) big bang, which is to say covering the whole population and the whole country in one go, (ii) starting with a population segment, usually the formal sector, in some countries simultaneously with the poor (creating the “missing middle” problem), or (iii) starting with a certain level of health provision, e.g. hospital care. In several cases, a combination of these sequencing approaches has been used.
Ghana opted for big bang, albeit based on its history with decentralized district Community-Based Health Insurance. Kenya has had a mandatory insurance mechanism for several decades for hospital care for government employees, which is now slowly morphing into a contributory scheme for all levels of care and the whole population. Tanzania has an insurance fund which started with government employees which later evolved to incorporate other population groups. Some countries which have more recently started to consider introducing health insurance have received advice to make them contributory, and to start with the whole population at once, as in Liberia and Sierra Leone, or by population group with the informal sector gradually being targeted, as in Lesotho. The experiences of the frontrunner sub-Saharan African countries, e.g. Ghana and Kenya, over the course of their early years should give one pause in thinking about sequencing.
Indeed, what we see in the schemes already in place is a significant set of difficulties with respect to getting off the ground, such as with the key components of governance, the benefits package, quality of services and financial protection. In Kenya, settling on a design and navigating towards a consensus, or simply setting aside the concerns of some interest groups, took years. There is also evidence that weak governance of the Kenya National Health Insurance Fund since it started transitioning to its larger role has prompted calls for reform. In Ghana, where membership has stagnated at between 30% and 40% of the population for several years, both those who can afford it, and even those who are exempt from paying premiums, do not sign up to the National Health Insurance Scheme (NHIS) for a multitude of reasons. A government committee recently studied the main causes of the challenges facing the Ghana NHIS and cited among five main flaws that many citizens cannot afford the contribution, quality of care is low, and that many facilities are unable to provide all the required benefits. There is evidence suggesting that rather than improving access, being an NHIS adherent relegates people to second class service, and that the cash and carry system, out of frustration for which the NHIS was born, lives on.
In the classic sequencing approaches (big bang, population, geography, level of service delivery), even those which target population groups or service delivery levels gradually, the management and governance infrastructure must be built up front. This poses two challenges. First that significant resources must be allocated to setting up and running the entire administration of national health insurance mechanisms (requiring investment in registering enrollees, getting them to pay premiums in contributory mechanisms, identification of the poor, claims management, software development or acquisition, handling insurance funds, contracting providers, running accreditation, etc), from the beginning. Second that the human resource capacity must be present from the start to run the various units of the purchaser. These are complex systems each of which deserves focus to get right.
Given the very serious and costly problems which peer countries in sub-Saharan Africa have faced in setting up the administration of national health insurance mechanisms, those countries taking serious looks at launching health insurance schemes should think soberly about a different way of sequencing.
A proposal for a component-based sequencing
As against the classic sequencing approaches there could be one based on health financing and service delivery components. Components in this sense is intended to refer to the various sub-components within the three main health financing functions (revenue generation, pooling, purchasing), as well as those within service delivery. This approach would build the various components needed for a national scheme in a step-wise and cohesive manner, starting by focusing on improving the supply of health services and building the purchasing function, before providing the public with an explicit entitlement and expecting them to pay. There is no defined way of implementing the sequencing, but there would be appropriate sequences based on the context, and logical requirements (some components need to come before others).
An example of such a sequencing would be to start with a very restrained purchasing arrangement and benefits package, and then move, in an order to be established based on context, through granting provider autonomy to public facilities (where it doesn’t exist), having the government contribute tax revenue and channeling donor funds to strategic purchasing, adding value-added information in the documentation requested from providers for payment, creating a single government health purchasing entity, accrediting providers, incorporating private providers, enforcing contract terms with providers including contract termination where needed, carefully thinking about increasing the number of services reimbursed through fee-for-service and / or having a capitation payment for non-salary operational costs run through the purchasing entity (rather than from the Ministry of Finance or the Finance Unit of the Ministry of Health), creating equity-based exemptions, enforcing gatekeeping, putting rules in place against balance billing and so on.
Regardless of the exact ordering in this approach, in contributory mechanisms, revenue generation from the population would be left towards the end, therefore leaving aside the complexities attached to premium collection, and conferment of an explicit entitlement to later in the process, once the purchasing and supply-side service delivery structures are able to respond.
There is of course a ready-made restrained purchasing arrangement already widely in place in sub-Saharan Africa, namely supply-side performance-based financing (PBF). The structures, processes and human expertise have been developed over the last decade in a large number of countries, including those now considering contributory health insurance. The proposal therefore would be to start with this scaled-down mechanism for, and therefore manageable starting point for, strategic purchasing.
The order of the sequencing by component, as well as the timing, are certainly up for discussion and depend on context. However there are several benefits in this line of thinking. First, a gradual build up by component is a much more manageable process to putting in place national health insurance than is an all-at-once approach. The latter would be complex for anyone to manage, let alone countries which don’t have the required capacity in numbers or skills. Second, this approach provides a clear roadmap for policy-makers, allowing them to focus on the key elements to build quality services, strategically purchased. Third, the build up by component is a much less expensive path administratively than is the all-at-once approach. Fourth, difficulties encountered along the way in building up by component will have fewer and less widespread ramifications than in an all-at-once approach. Fifth, that building up by component can take as its starting point a pre-existing small-scale purchasing arrangement which is already widely present across sub-Saharan Africa. Sixth, that in this approach, the foundation for strategic purchasing is built at the start, preventing problems as seen in some countries in building strategic purchasing into insurance later on. Seventh, that in contributory mechanisms, leaving revenue generation from the population to later in the process gives the government more time to focus on improving both the purchasing function and the supply of health services, before adding into the mix the administratively expensive and complex, and politically charged, activities related to providing the population with an explicit entitlement, and asking them to pay for it. And eighth, this approach is inherently more equitable than the classic approaches, in the sense that in contributory mechanisms, without the need to collect premiums until later in the process, the system is not improved only for, or access only improved for, those who can afford the premiums.
I am humbly proposing this approach to help low and lower-middle income countries transition from passive to active purchasing more manageably. There are doubtless many issues to be thought through in this approach which I have not highlighted in this blogpost. I would be very happy to read reactions and suggestions for making this approach more robust.
A Collectivity Project is coupled to this blog. If you comment the blog, you are contributing to the project and are eligible for a participation badge.